“A Multidisciplinary Approach is Best for Stargardt’s Disease”, IALVS
Diana Shechtman, OD, FAAO & Marc Gannon, OD, FAAO, FIALVS with Richard J. Shuldiner, OD, FAAO, FIALVS, Chief Clinical Editor
When you think nothing more can be done, tell the patient to Google “low vision help”.
Case
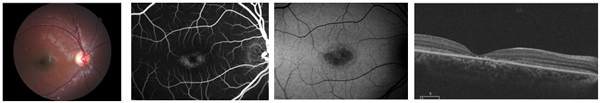
An 8-year-old Hispanic male presented to me, Dr. Shechtman, with decreased vision OU. BCVA was 20/200 OD, OS. Patient had an unremarkable ocular, medical and family history. Pupils, EOMs, confrontation fields, and color vision were all normal.DFE showed granular deposits in the maculae OU correlating to severe macular thinning on SDOCT OU. Additionally, a disrupted RPE/PIL has denoted subfoveal OU. MfERG showed impaired foveal function, while FAF showed increase autofluorescence parafoveally with central hypofluorescence (Bull’s eye appearance) OU, correlating with loss of RPE integrity. FA revealed the classic dark choroid.
The patient was diagnosed with Stargardt’s Disease. Genetic counseling was offered, and the patient was scheduled with a low vision (LV) specialist to discuss LV options and educate the parents/school regarding the patient’s needs. Information was also provided regarding diet, whereby high levels of vitamin A should be diminished.
What Is Stargardt’s Disease?
Although encountering a patient with Stargardt’s Disease (SD) is infrequent, SD is the most common form of inherited macular dystrophy. It is a lipofuscin storage disease, which affects the RPE/photoreceptors through a sequence variant in ABCD4 gene.
Stargardt’s Disease is characterized by bilateral macular atrophy, described as “a beaten bronze appearance” in the end-stage. Stargardt’s Disease may present with or without classic disciform-shaped yellow retinal flecks throughout the posterior pole. The young patient with SD will experience progressive central severe vision loss which stabilizes by young adulthood. Clinical findings are subtle during the first decade of life. Hence, using a multitude of diagnostic modalities is best to confirm the diagnosis. Such tests include, but are not limited to, fundus photography, FA, FAF, mfERG and genetic testing. There is no current standard treatment although ongoing clinical trials are looking into the benefits of stem cell therapy, gene replacement therapy, and pharmacological approaches.
A multidisciplinary approach in management includes working with distinct specialists to confirm the diagnosis and address the patients’ visual needs. Such a multidisciplinary approach often yields the best management for visual function. I referred this patient to a low vision optometrist.
Options in Low Vision Rehabilitation in Ft. Lauderdale
Stargardt’s Disease, like Macular Degeneration, results in compromised central visual function. It is most important in these patients to initially assess the central acuity and establish the visual goals and needs of the patient. In the earlier stages, acuities of 20/60 or better are frequently found. In this case the patient may benefit from accurate central refraction, assuming the distant requirements in the classroom or office are adequately met by this level of acuity.
If near point tasks require better than 20/60, simple magnification in the form of high-powered bifocals or prism readers may fulfill the job. With VA in the 20/70 to 20/100 range, central fixation is still possible, but more magnification is needed. This can take the form of microscope glasses for near or telescopic glasses that can be focused for specific tasks at any distance.
The Stargardt’s patient, in this case, has central acuities of 20/200 OU. Whenever best central acuity is 20/100 or less, it becomes necessary to test eccentric acuity and evaluate the residual function that may exist in para-central and peri-central areas of the retina. This is best done dynamically at distance using a target that can be easily moved, such as the Designs for Vision Feinbloom Acuity Chart. Once the areas of function are identified, then their relative size and sensitivity need to be established.

In the case of this SD patient, the fixation in each eye was 10 degrees to the right of center. Armed with this information, I performed a refraction at these most functional eccentric areas which yielded the best level of acuity. This refraction was different from the central refraction. One can expect acuities to be, typically, 3 to 5 times better than the central acuity.
In our patient, the eccentric acuities OU were 20/60 and thereby he responded to the same levels and types of magnification that our central patients would use. However, the big difference here is that the patient had to be taught/trained to view eccentrically. With that being accomplished, with or without the low vision device, the patient was able to enjoy the same levels of function that the centrally fixating patient would otherwise be capable of as well.
This 8-year-old student has needs at distance, at near-point (reading), and intermediate (computer) ranges. It became necessary to explore various aids such as portable CCTV’s, magnifiers, telescopes, and tele-microscopes to meet his needs.
In this case, a viable solution was a trioptic ocular system, a pair of glasses with a Bioptic telescope mounted in the top for distance function and a microscopic bifocal for near point function, with an intermediate ribbon/carrier lens containing his distant Rx. This provided him a “hands-free” option enabling him to function fluidly at multiple ranges in a classroom setting.

Conclusion
Patients with ocular conditions which might lead to vision loss require at least two eye care professionals: one to treat the medical condition, if treatments are available, and one to treat the vision loss condition to keep the patient functioning. While most have the belief that one eye care provider can handle both issues, we know that this is not the case.
In the above described case, the ocular condition, Stargardt’s Disease, has no cure or treatment. In other conditions, such as wet ARMD or diabetic retinopathy, medical treatments are available to limit the vision loss. However, once vision is lost, standard of care dictates referral to an experienced low vision rehabilitation provider.